Definition & Overview
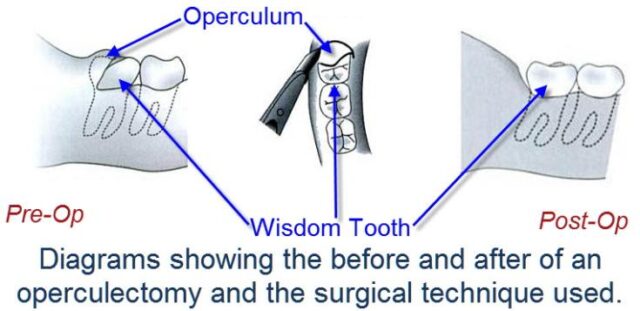
Operculectomy is the surgical procedure of removing the operculum, or the flap of gum that partially covers a tooth. This procedure is done to treat pericoronitis, a condition characterised by pain and inflammation of the operculum. Pericoronitis typically occurs among young adults, especially those whose wisdom tooth is starting to erupt.
The dental operculum is a mass of soft tissue found on a partially erupted tooth. It is most commonly associated with lower wisdom teeth though it can also be seen covering the permanent molars and some baby teeth. It is quite apparent when a tooth begins to erupt and peek through the gum tissue. In normal circumstances, the gum tissue recedes as the tooth continues to erupt and moves into its proper position. A fully erupted tooth should no longer have any flap of gum tissue on its chewing surface.
In the case of the lower wisdom teeth, there is typically little to no space left for the tooth to fully erupt and come out of the gum line. As such, the operculum over the wisdom teeth does not fully recede and could permanently cover the affected tooth. The presence of operculum sometimes causes oral health issues. There is an increased chance of biting the closely adjacent cheek tissue or the operculum itself. Tooth decay is also another possibility since it is quite difficult to clean the area underneath the gum. This condition could develop even if proper oral hygiene is practiced. The upper molars could also cause pressure on their lower counterpart, causing pain. This might impact the patient’s quality of life, as eating becomes a painful activity.
Who Should Undergo and Expected Results
Patients suffering from acute pericoronitis or operculitis are suitable candidates for operculectomy. This condition is characterised by sudden onset of inflammation of the operculum, causing pain and discomfort. Symptoms of acute pericoronitis include swelling of the gum tissue, fever, and accumulation of pus in the affected area. If left untreated, the disease can also cause other systemic complications such as swollen lymph nodes, weakness, and general malaise. The pain may also travel to other parts of the face, such as the ear, jaw, and the floor of the mouth. It can also cause pain in the throat. Extreme cases of acute pericoronitis may even affect diet, as the patient may find it difficult to chew food or even open their mouth.
Those who have chronic pericoronitis may be offered operculectomy to prevent the expected worsening of symptoms and avoid pain. Chronic pericoronitis is characterised by recurring inflammation of the operculum. In some cases, the patient may feel no symptoms at all. However, there may still be pain and swelling in the gum tissue. The presence of bacteria during these chronic episodes may also lead to halitosis or bad breath. In some cases, chronic pericoronitis could be a precursor to the development of paradental cysts.
Operculectomy is a relatively simple and safe procedure with good success rates. Patients usually achieve immediate relief from pain and discomfort. The further buildup of plaque or tartar is also prevented. Patients will also find it easier to keep this area of the mouth clean. If the tooth has not been impacted, the removal of the operculum will encourage it to fully erupt.
The patient is advised to rest for several days after surgery and to adhere to soft food diet while waiting for the gum tissue to heal. A follow-up check with the dentist is also mandatory to ensure that no complication has occurred and the tissues are healing well.
How is the Procedure Performed?
The patient is given local anaesthesia prior to surgery. The dentist then makes one or more incisions on the operculum, loosening the flap on top of the affected tooth. Using a scalpel, the dentist then proceeds to excise the gum tissue. The dentist can also use a radio-surgical loop to remove the operculum. The wound is then closed with sutures, or the dentist can leave it open to heal by itself.
Operculectomy can also be performed using electrocautery. A small probe is placed on the surgical site, and mild electric current is transferred into the tissue. The heat resulting from the alternating current can cause the soft tissue of the operculum to disintegrate. This allows the dentist to cut through and remove the gum tissue covering the chewing surface of the tooth. No dressing is required for this procedure.
A dentist can also use diode laser to perform the removal of an inflamed operculum. The most common type of laser used in this procedure is carbon dioxide laser. Following the administration of local anaesthesia, the handpiece of the laser is held near the target tissue. Using laser pulses, the target tissue is ablated. The dentist has to make sure that the enamel of the tooth is not hit by the laser pulse to avoid tooth damage. Once all the operculum tissue has been removed, and haemostasis has been achieved, the handpiece is slowly moved out of the surgical site. The wound is left open to heal by itself.
Other techniques for treating pericoronitis include the use of caustic agents like trichloroacetic acid and cryosurgery. The caustic agent is placed under the operculum to dissolve the soft tissue in a controlled manner. Cryosurgery involves subjecting the operculum to extreme cold temperature to induce tissue necrosis. The dentist can then use a scalpel to remove the dead tissue.
Possible Risks and Complications
The biggest risk associated with operculectomy is the potential damage to the lingual nerve, which is responsible for supplying sensation to the tongue. An injury could mean the patient would be unable to perceive taste when eating or drinking. In some cases, numbness to the tongue could also be experienced. This complication may resolve itself over time or may become permanent. There is also the possibility of bleeding and infection. Infection could also travel to the blood stream, causing sepsis. This is a potentially dangerous complication, since the surgical site is near the brain. Also, there is a possibility that the operculum could regrow and become infected again. This would necessitate another treatment session.
Reference:
- Dodson TB (Sep 2012). “The management of the asymptomatic, disease-free wisdom tooth: removal versus retention. (review)”. Atlas Oral Maxillofac Surg Clin North Am. 20 (2): 169–76